Medicare Care Management: A Rural Clinic Roadmap
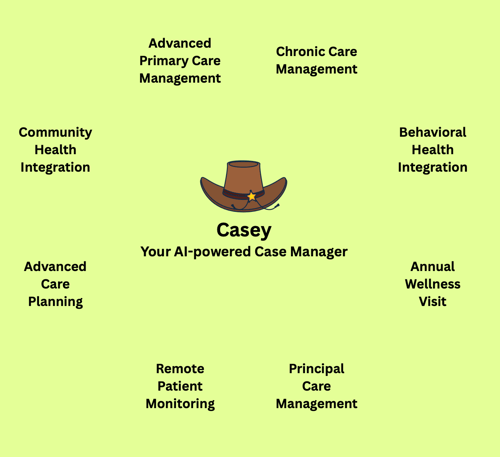
Rural communities face unique healthcare challenges like staff shortages, geographic barriers, and limited resources, often leaving patients with multiple chronic conditions underserved. Fortunately, Medicare has recognized the vital role of care management in improving outcomes and reducing costs. From Chronic Care Management (CCM) to Behavioral Health Integration (BHI) and beyond, there are eight distinct Medicare care management pathways. For Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs), understanding how to deliver and bill these services is essential.
In this post, we will:
- Provide a high-level overview of Medicare’s eight care management programs (2011–2025).
- Deep dive into chronic care management (CCM) specifically for RHCs/FQHCs current billing (G0511) and the January 1, 2025 transition to standalone CPT codes (99490, 99487, etc.).
- Showcase how an AI Case Manager like Casey can streamline patient identification, documentation, and billing, ensuring no eligible minute (or dollar) is left on the table.
1. Medicare’s Eight Care Management Programs (2011–2025)
Over the past decade-plus, Medicare has incrementally introduced new care management codes to encourage proactive, non–face-to-face coordination and support for high-risk patients. Below is a concise rundown of each program, its launch year, key codes, and who can furnish them:
- Annual Wellness Visit (AWV) – 2011
- Codes:
- G0402: “Welcome to Medicare” initial preventive physical exam (Electronic Health Risk Assessment included)
- G0438: Initial AWV (first annual wellness visit after IPPE)
- G0439: Subsequent AWV (yearly update)
- + Preventive Screening Codes: G0442/G0443 (alcohol misuse screening & brief counseling), G0445 (STI counseling), G0446 (cardiovascular counseling), G0447 (obesity counseling), G0101/G0102 (pelvic/breast & prostate exams), 99406/99407 (tobacco cessation).
- Who Furnishes: Physician or qualified non-physician practitioner (NP/PA).
- Why It Matters: AWVs are 100% preventive, with no patient cost-sharing. Clinics performing AWVs can identify patients who may benefit from additional care management down the road (e.g., CCM, BHI).
- Codes:
- Chronic Care Management (CCM) – 2015
- Codes:
- 99490: Non-complex CCM, 20 minutes/month of clinical staff time under a provider’s supervision (patients with ≥2 chronic conditions).
- 99439: Add-on for each additional 20 minutes of non-complex CCM.
- 99487: Complex CCM, 60 minutes/month of clinical staff time (moderate/high complexity).
- 99489: Add-on for each additional 30 minutes of complex CCM.
- 99491: Physician/QHP-provided CCM, 30 minutes/month (no clinical staff credited).
- 99437: Add-on for each additional 30 minutes of physician/QHP time.
- Who Furnishes: Billed by a physician or other qualified practitioner (MD, DO, NP, PA) but largely performed “incident to” by clinical staff (RNs/LPNs) under general supervision, except 99491/99437, which are personally furnished by the provider.
- Why It Matters: CCM helps clinics coordinate care for high-need patients, reduce avoidable hospitalizations, and offset staffing shortages by reimbursing non–face–to–face activities.
- Codes:
- Advance Care Planning (ACP) – 2016
- Codes:
- 99497: Advance care planning, first 30 minutes, face-to-face.
- 99498: Each additional 30 minutes of ACP (add-on).
- Who Furnishes: Physician or qualified health professional (NP/PA, social worker in some contexts).
- Why It Matters: Documenting patient goals and advance directives not only improves patient-centered care but is separately reimbursed when done alongside an AWV.
- Codes:
- Behavioral Health Integration (BHI) – 2017
- Codes:
- 99484: General BHI, ≥20 minutes/month by clinical staff (no psychiatric consultant required).
- G0323: BHI services, 20 minutes by a clinical psychologist or clinical social worker.
- Who Furnishes: 99484 is billed by a physician/QHP and furnished by clinical staff (e.g., behavioral care manager); G0323 is billed and furnished by a psychologist or social worker.
- Why It Matters: Integrating mental health support into primary care is critical for rural populations facing stigma and access barriers.
- Codes:
- Remote Patient Monitoring (RPM) – 2019
- Codes:
- 99453: RPM device setup & patient education (one-time per device).
- 99454: Supply of RPM device with daily data transmission (per 30 days; ≥16 days of data required).
- 99457: RPM treatment management services, first 20 minutes of provider time per month (includes at least one interactive communication).
- 99458: Add-on for each additional 20 minutes of RPM management.
- 99474: Self-Measured Blood Pressure (SMBP) services (30 days) data interpretation.
- 99091: Data interpretation & ≥30 minutes of provider time (older RPM code, not billable with 99457/99458 in the same month).
- Who Furnishes: Billed by physician/QHP; time may be furnished by clinical staff under supervision (except for 99091, which must be performed by the billing provider).
- Why It Matters: RPM expands care reach across distance, which is critical when broadband and travel are limited in rural areas.
- Codes:
- Principal Care Management (PCM) – 2020
- Codes:
- 99424: PCM for one complex chronic condition, 30 minutes/month, personally furnished by the provider.
- 99425: Add-on 30 minutes for physician/QHP time.
- 99426: PCM, 30 minutes/month by clinical staff under supervision (for one chronic condition).
- 99427: Add-on 30 minutes for clinical staff time (PCM).
- Who Furnishes: Billed by the provider; services furnished either personally by the provider (99424/99425) or by clinical staff under their supervision (99426/99427).
- Why It Matters: PCM covers the management of a single high-risk condition, leaving room for RHCs/FQHCs to carve out resources for their sickest patients.
- Codes:
- Remote Therapeutic Monitoring (RTM) – 2022
- Codes:
- 98975: RTM device setup & patient education (one-time).
- 98976/98977: Supply of RTM device for respiratory (98976) or musculoskeletal (98977) data monitoring (per 30 days; ≥16 days data).
- 98980: RTM treatment management, first 20 minutes/month.
- 98981: Add-on for each additional 20 minutes of RTM management.
- Who Furnishes: Billed by physician/QHP (MD/DO/NP/PA/PT/OT); services can be furnished by clinical staff or auxiliary therapists under supervision.
- Why It Matters: RTM supports chronic pain, respiratory disease, and other conditions, offering a new avenue for distance-based rehabilitation or pain management.
- Codes:
- Community Health Integration (CHI) – 2024
- Codes:
- G0019: CHI services, 60 minutes/month by trained auxiliary personnel (e.g., community health worker) under the general supervision of a billing provider.
- G0022: Each additional 30 minutes of CHI (add-on to G0019).
- Who Furnishes: Billed by a physician or qualified practitioner (NP, PA, CNM); services delivered by auxiliary personnel (community health workers, social service coordinators, etc.).
- Why It Matters: CHI is built for Social Determinants of Health (SDOH) to support exactly the kind of wraparound care essential in resource-limited rural settings.
- Codes:
2. Chronic Care Management (CCM) for RHCs & FQHCs: Today’s Approach (G0511)
2.1. Why RHCs/FQHCs Use G0511 Instead of 99490/99487 Today
From January 1, 2018, until December 31, 2024, Rural Health Clinics and FQHCs have billed a single “catch‐all” code, G0511 (“General Care Management”), whenever they deliver any type of CCM, BHI, PCM, or related care management services to an eligible Medicare patient. Instead of choosing among 99490, 99487, or 99484, they simply bill G0511 once per patient per calendar month. CMS sets the G0511 reimbursement each year as an average of the non‐facility Physician Fee Schedule (PFS) rates for those codes.
- 2024 G0511 Payment Range: Approximately $72.98 – $80.56 per patient per month, depending on geography.
- What’s Covered: Non‐complex CCM (99490), complex CCM (99487), Behavioral Health Integration (99484), and selected add-on activities.
- Who Bills & Who Furnishes:
- The RHC/FQHC’s billing practitioner (MD/DO/NP/PA/CNM) must be enrolled in Medicare under the clinic’s site number; that individual’s NPI shows on the claim.
- Clinical staff (RN/LPN/LCSW, etc.) can perform the non–face-to-face tasks: medication reconciliation, referral follow-up, SDOH needs assessment, etc., under the general supervision of the billing practitioner.
2.1.1. Patient Eligibility & Enrollment
- Medicare Part B Beneficiaries with two or more chronic conditions expected to last ≥12 months (or until death).
- An initial face-to-face visit is required. This could be any billable E/M or preventive visit (e.g., AWV, office visit). During that encounter, the billing practitioner:
- Explains the CCM benefit (20+ minutes of non–face-to face coordination each month, 20% coinsurance applies).
- Obtains and documents verbal (or written) patient consent.
- Creates a Comprehensive Care Plan (CCP), including diagnoses, current medications, providers, functional status, goals, and advance directives.
- Ongoing CGM (Cumulative Non–Face-to-Face Activity)
- Throughout the month, clinical staff track cumulative time spent on care management tasks (in 20-minute increments).
- Documentation can live in EHR flowsheets, progress notes, or case management logs.
- Monthly Billing
- Once the patient’s chart shows ≥20 minutes of CCM activity, the clinic submits G0511 on the next RHC/FQHC facility claim.
- If G0511 is provided on the same date as another billable RHC/FQHC visit, CMS pays whichever is higher, only one payment per date of service.
2.2. Limitations & Operational Workarounds
- Single Monthly Payment: Even if a patient requires 60 or 80 minutes of CCM, RHCs/FQHCs only receive one flat G0511 payment, and there’s no “add-on” for additional time.
- Bundling: If the patient also qualified for BHI or PCM in the same month, RHCs/FQHCs still bill only G0511 (BHI-specific codes cannot be billed separately).
- Documentation Burden: Clinics must carefully track minutes and ensure the CCP is updated monthly. If even one box is unchecked, no documented consent or no completed CCP, CMS may deny G0511.
Operational Tip: Using a platform that automates time-logging, generates real-time “Minutes Tracker” alerts, and surfaces missing care plan elements (like Casey) can dramatically reduce denials and revenue leakage.
3. The Big Shift: Individual CCM Codes in RHC/FQHC Claims (January 1, 2025)
Starting January 1, 2025, RHCs and FQHCs can abandon G0511 in favor of the specific PFS CPT codes, just as a traditional provider would. Instead of an all-in-one bundled rate, they can bill:
- Non-Complex CCM:
- 99490 (20 minutes of clinical staff time/month)
- 99439 (each additional 20 minutes of non-complex CCM)
- Complex CCM:
- 99487 (60 minutes of clinical staff time/month, moderate/high complexity)
- 99489 (each additional 30 minutes of complex CCM)
- Physician-Delivered CCM:
- 99491 (30 minutes/month personally provided by provider)
- 99437 (each additional 30 minutes of provider time/month)
3.1. Why This Matters
- Precision Reimbursement
- Instead of a “one-size-fits-all” G0511 rate, RHCs/FQHCs now receive the full non-facility PFS rate for whichever CPT code they bill.
- Example: If a clinic performs exactly 20 minutes of non-complex CCM in April, they bill 99490 and receive roughly $61. If they perform 40 minutes, they bill 99490 + 99439 for roughly $108.
- Ability to Capture Complexity
- Complex patients (those needing ≥60 minutes of coordination or higher decision-making) can generate higher reimbursement under 99487 + 99489 (total potentially $203+ for 90 minutes in one month).
- Against G0511’s flat $75–$80, that difference can be transformative for a rural clinic’s bottom line.
- Maintain RHC/FQHC Claim Structure
- Even though they’re billing CPT codes, RHCs/FQHCs still submit care management services on CMS-1450 (UB-04) facility claims under the Part B section. That means they still benefit from RHC/FQHC-specific payment rules (e.g., “all or none” payment on a single date of service).
3.2. Updated Workflow for RHCs/FQHCs (Starting 1/1/2025)
- Patient Identification & Enrollment
- Identify Medicare Part B patients with ≥2 chronic conditions (via an EHR registry or platform like Casey).
- Ensure the patient has signed consent and a valid CCP on file before any non–face–to–face work begins.
- Comprehensive Care Plan (CCP) Creation
- On the first face-to-face visit (e.g., AWV, new patient exam), the billing practitioner (MD/NP/PA) documents the CCP in the chart listing problems, medications, providers, goals, SDOH needs, and advance directives.
- Casey can auto-populate a CCP template by scanning the patient’s problem list, medication list, and recent labs, then prompt the provider to verify or adjust.
- Monthly Non-Face-to-Face Service Delivery
- Clinical staff (e.g., RN care manager, LPN, or behavioral health coach) deliver CCM tasks: med reconciliation, care coordination, lab follow-up, patient outreach, social determinant screenings, etc.
- Each task is timestamped; Casey tallies the total minutes per patient in realtime (e.g., 22 minutes → eligible for 99490; 65 minutes → eligible for 99487).
- Provider-Delivered CCM (If Applicable)
- If the billing practitioner personally spends time (e.g., reviewing records, consulting with specialists, speaking directly with the patient by phone), they can document that time as 99491 (first 30 minutes) or add 99437 for additional 30-minute increments.
- Casey highlights “provider-provided minutes” versus “clinical staff minutes” so the clinic can choose the most appropriate code mix.
- Monthly Claim Preparation
- At month’s end, the billing team using Casey’s autogenerated report sees, for each patient:
- Total clinical staff minutes (which codes apply: 0–19 min = none; 20–59 min = 99490; 60+ min = 99487 plus 99489 if >90 min).
- Total provider minutes (30 min increments → 99491 + 99437 add-ons).
- Clinic staff verify that consent is in the chart, the CCP is updated, and the notes meet documentation guidelines.
- They insert codes (e.g., 99490, 99439 | 99487, 99489 | 99491) on the RHC/FQHC claim.
- At month’s end, the billing team using Casey’s autogenerated report sees, for each patient:
- Bill and Track Coinsurance
- Patients owe 20% coinsurance on these CPT codes.
- Clinics can track whether patients have supplemental coverage (Medigap, Medicare Savings Programs) that may waive that coinsurance. Casey can flag at-risk patients (e.g., known to have “Dual Eligibility,” so cost-share is $0).
- Avoid Overlapping Visits
- If CCM codes are the only service on a given date, they’re paid in full. If there is another billable RHC/FQHC encounter that day (e.g., a sick visit), only one code (typically the higher-valued E/M or CCM code) will pay. Casey can alert schedulers if a CCM patient tries to check in “for a sick visit” on the same date as their CCM services.
- If CCM codes are the only service on a given date, they’re paid in full. If there is another billable RHC/FQHC encounter that day (e.g., a sick visit), only one code (typically the higher-valued E/M or CCM code) will pay. Casey can alert schedulers if a CCM patient tries to check in “for a sick visit” on the same date as their CCM services.
4. A Closer Look at Chronic Care Management Steps for RHCs/FQHCs
Below is a more detailed, step-by-step guide to delivering CCM in a rural clinic setting, first with G0511 (2024 and earlier) and then CPT codes (2025 onward).
4.1. Today (G0511 Workflow, Through 12/31/2024)
- Identify Eligible Patients
- Use EHR filters or a built-in registry to find Medicare Part B beneficiaries with two or more chronic conditions (e.g., diabetes, CHF, COPD, dementia).
- Pull a “CCM candidate list” monthly to track which patients have not yet been enrolled in CCM.
- Obtain Patient Consent
- During a face-to-face appointment (e.g., Annual Wellness Visit, chronic disease follow-up), the billing practitioner (physician, NP, or PA) educates the patient about:
- CCM services (non–face-to-face coordination for 20+ minutes per month).
- 20% coinsurance responsibility.
- Document verbal or written consent in the medical record (date, patient signature or spoken affirmation, name of the person who discussed).
- During a face-to-face appointment (e.g., Annual Wellness Visit, chronic disease follow-up), the billing practitioner (physician, NP, or PA) educates the patient about:
- Create a Comprehensive Care Plan (CCP)
- Still during that initial encounter (or within 30 days), the billing practitioner completes a discrete CCP:
- Lists chronic diagnoses, active medications, and specialty providers involved.
- Documents functional status (mobility, ADLs), SDOH concerns (food/housing insecurity), advance directives, and patient self-management goals.
- Store the CCP in a designated EHR section for easy monthly updates.
- Still during that initial encounter (or within 30 days), the billing practitioner completes a discrete CCP:
- Deliver Non–Face-to-Face Services (≥20 Minutes/Month)
- Within the next month, clinical staff perform:
- Medication reconciliation (ensuring patient understands dosages, checking for interactions).
- Lab/radiology follow-up (calling to schedule or review results).
- Outreach calls (checking on patient’s progress or side effects).
- Social Determinant screenings (food access, transportation needs).
- Documentation in progress notes or a CCM-specific flowsheet and record actual minutes spent on each task.
- Within the next month, clinical staff perform:
- Track Minutes & Documentation
- Staff must tally cumulative minutes (in 20-minute blocks). If they reach at least 20 minutes, the patient becomes billable for G0511.
- Clinic leadership should audit time logs weekly; missed minutes or if a nurse only logs 15 minutes means the clinic can’t bill G0511 that month.
- Submit G0511 on Monthly Claim
- Typically on the first RHC/FQHC claim submission of the month, the clinic adds G0511 to every patient who hit 20 minutes of documented time (and who had a valid CCP and consent).
- CMS pays a flat rate (e.g., $75–$80) per patient. If the same patient had a billable sick visit or immunization that day, the higher-paying service would be paid; otherwise, G0511 is paid as a standalone.
- Repeat Each Month
- Enrollment and consent only need to be done once unless the patient revokes.
- CCP must be reviewed and updated monthly, documenting any changes in health status, new medications, or revised goals.
- Every 30 days, the clinic ensures 20 minutes of non–face-to-face work happens, documents it, and bills G0511.
4.2. Beginning January 1, 2025 (CPT Code Workflow)
Key Difference: Instead of billing G0511, RHCs/FQHCs choose precise CPT codes that reflect the actual time and complexity of CCM services delivered.
- Patient Identification & Consent
- Exactly the same: find Medicare Part B patients with ≥2 chronic conditions, obtain and document consent during a face-to-face visit, and create/update a CCP.
- Document & Tally Minutes
- Clinical staff continue to perform non–face-to-face tasks each month. Casey or another tool can auto‐aggregate total minutes by the patient.
- If clinical staff accumulate:
- 20–59 minutes → bill 99490 (≈ $61)
- ≥ 60 minutes → bill 99487 (≈ $132) + use 99489 ($71 each extra 30 minutes) if they exceed 60 minutes (e.g., 90 minutes = 99487 + 99489 for roughly $203).
- Include Provider-Delivered Minutes
- If the billing practitioner personally spends non–face-to-face time (e.g., 30 minutes telephoning a specialist or reviewing records), these minutes can be billed as 99491 ($82 for the first 30 minutes) or 99437 ($59 for each additional 30 minutes).
- Example:
- A physician spends 45 minutes a month reviewing labs and adjusting medications (no clinical staff involvement). That physician can bill 99491 ($82) + 99437 ($59) = $141.
- If that same 45 minutes by the physician is paired with 20 minutes of RN work, the clinic could bill 99491 ($82) + 99490 ($61) = $143, whichever combination yields a higher total payment.
- Claim Submission Process
- On the RHC/FQHC claim form (CMS-1450), list the CCM CPT codes in the Part B section.
- If a CCM code shares a date of service with a billable RHC/FQHC outpatient visit (e.g., a diabetes follow-up), the calendar date can only pay one code, and the higher-valued service typically wins.
- If CCM is the only service that day, it pays in full.
- Coinsurance & Reconciliation
- Patients are responsible for 20% of the allowed amount for each CPT code. RHCs/FQHCs should track which patients have supplemental coverage (e.g., Medicaid for “Dual Eligibles”) so coinsurance is waived or billed appropriately.
- Billing staff reconciles at month end to ensure each patient’s chart had:
- Valid consent on file,
- CCP updated in the last 30 days,
- Documentation of minutes to meet the billed code(s).
- Ongoing Care Plan Updates
- Each month’s face-to-face or virtual check-in provider reviews (or Casey summarizes) any new data (lab results, remote monitoring readings, patient-reported outcomes).
- The CCP is updated to reflect new diagnoses, medication changes, or revised goals (e.g., “Patient’s HbA1c is now 8.2%, adjust diabetic management plan”). Casey can auto‐craft a “CCP draft” for providers based on EHR data.
5. How an AI Case Manager (Casey) Makes CCM Easier for RHCs/FQHCs
Delivering CCM at scale in a rural clinic where staff are stretched thin and patients may live hours away can feel overwhelming. This is where an AI Case Manager like Casey can be a game-changer. Here’s how Casey streamlines every step:
- Automated Patient Identification
- Casey scans the EHR nightly for Medicare Part B patients with ≥2 chronic conditions who aren’t enrolled in CCM yet.
- Generates a “CCM Candidate List” and sends alerts to care coordinators to schedule face-to-face enrollment visits.
- Consent & Care Plan Templates
- Instead of providers manually typing a CCP, Casey auto-populates a template:
- Pulls active problem lists, current medication data, lab results, last AWV findings, social determinant flags, and existing advance directives.
- Providers review and finalize in a few clicks so the required CCP is complete within minutes.
- Instead of providers manually typing a CCP, Casey auto-populates a template:
- Real-Time Time Tracking & Alerts
- When a nurse or care coordinator completes a CCM task (e.g., calling the patient about medication side effects), they log a brief note in the Casey Care Platform. Casey automatically timestamps and sums “minutes spent” by the patient.
- Once a patient hits 20 minutes (for 99490) or 60 minutes (for 99487), Casey sends an alert: “John Doe has 22 minutes of documented CCM ready to bill 99490.”
- If a billing practitioner logs non-face-to-face time, Casey distinguishes that from staff time, ensuring accurate selection between 99490/99487 vs. 99491.
- Comprehensive Care Plan Maintenance
- Each month, Casey reviews patient data (new labs, imaging, EKGs, remote monitoring metrics) and drafts recommended CCP updates, “HbA1c rose from 7.8% to 8.4%.”
- The provider or NP simply reviews signs off, and moves on. No more hunting through charts.
- Billing Roster & Claim Preparation
- At month’s end Casey creates a billing roster listing:
- Each enrolled patient,
- Total staff minutes, total provider minutes,
- Codes to bill (e.g., 99490 + 99439 or 99487 + 99489, or 99491 + 99437),
- Whether consent & CCP are up to date.
- Billing staff reviews Casey’s roster, confirms everything is in order, and exports CPT codes to insert on the RHC/FQHC claim.
- At month’s end Casey creates a billing roster listing:
- Patient Engagement & Adherence
- Casey sends automated SMS/email reminders to CCM-enrolled patients:
- “Hi, Mrs. Martinez, Just checking in on your medication refill for metformin. Reply 1 if you need help.”
- “Tomorrow is your telephonic diabetes check-in. Please be ready for a 10-minute call.”
- Response data (e.g., “I ran out of insulin”) is routed to the care team for immediate follow-up, ensuring continuous engagement and reducing adverse events.
- Casey sends automated SMS/email reminders to CCM-enrolled patients:
- Reporting & Quality Insights
- Casey’s dashboard highlights which patients haven’t had any CCM activity in 30 days, which ones need CCP updates, and geographic clusters of high-risk patients.
- RHC/FQHC leadership can use these insights to allocate staffing (e.g., “Our highest CCM gap is among COPD patients in the northeast service area; assign an RN case manager to focus there”).
6. Putting It All Together: A Hypothetical RHC Workflow
Scenario: Pine Valley Rural Health Clinic (RHC) serves a mostly Medicare population scattered across 50 miles of farmland. They’re committed to starting CCM for their highest-risk patients but haven’t yet automated their processes. Here’s how Casey helps them execute:
- Week 1 (December 2024)
- Casey identifies 45 Medicare Part B patients with ≥2 chronic conditions who haven’t received CCM.
- The care team prioritizes the top 10 highest-risk patients (based on last hospitalization, A1c > 8.0%, or frequent ED visits).
- During routine visits in Week 1, the NP enrolls 10 patients in CCM, obtaining verbal consent and signing the initial CCP (drafted by Casey).
- Month of January 2025 (First Month of CPT Codes)
- Throughout January, Casey tracks all CCM tasks:
- RN spends 25 minutes on Mr. Thompson (med reconciliation, lab coordination) → alert to bill 99490.
- Case Manager spends 65 minutes on Ms. Lopez (complex care: social service referral, specialty appointment scheduling, SDOH screening) → alert to bill 99487 (60 min) + 99489 (additional 30 min) = $203.
- NP spends 35 minutes telephoning high-risk patients → alert to bill 99491 (30 min) + 99437 (additional 30 min) = $141.
- At month’s end, Casey’s “CCM Billing Roster” shows each patient’s code allocation and confirms that consent & CCP are current.
- Throughout January, Casey tracks all CCM tasks:
- Billing January 2025
- Pine Valley inserts these codes on their RHC claim:
- Mr. Thompson: 99490 ($61)
- Ms. Lopez: 99487 ($132) + 99489 ($71)
- Dr. Patel’s “provider-driven CCM” patients: 99491 + 99437 as needed
- The claim is submitted, and Pine Valley collects 20% coinsurance from commercially insured patients; patients with a Medicare Savings Program have no coinsurance.
- Pine Valley inserts these codes on their RHC claim:
- Month of February 2025 and Beyond
- Casey re-analyzes labs, medication refill data, and remote monitoring results (if any).
- It flags patients who have dropped below 20 minutes of CCM activity (e.g., “Mrs. Miller has only 10 minutes in February; set up a follow-up call”).
- Care team adjusts workflows:
- Adds a mid-month “CCM huddle” where an RN proactively reaches out to any patient who has fewer than 15 minutes of tasks documented.
- At month’s end, the billing roster is ready again, no chart mining is required.
7. Key Takeaways for RHCs & FQHCs
- Now (Through 7/1/2025):
- Bill G0511 once per patient per month, regardless of non-complex, complex, or behavioral health integration tasks.
- Rate is a fixed average (~$75–$80), so high-need patients often “out-earn” low-need patients.
- Critical to document 20+ minutes, maintain a valid CCP, and secure consent.
- Starting 1/1/2025:
- Bill specific CCM CPT codes (99490/99439 for non-complex; 99487/99489 for complex; 99491/99437 for provider-driven) on the RHC/FQHC claim.
- Each code pays the full non-facility PFS rate, giving clinics an opportunity to better align reimbursement with actual time/effort.
- Claims must still follow RHC/FQHC facility rules (only one payment per date of service; CPT codes inserted in Part B lines).
- Operational Best Practices:
- Use an EHR registry or AI-enabled platform (like Casey) to:
- Identify eligible patients and track those not yet enrolled in CCM.
- Automate time tracking for any non–face-to-face tasks (RN, case manager, PAs).
- Generate and update CCPs each month to meet documentation requirements.
- Produce an end-of-month billing roster with the exact CPT codes to submit.
- Alert staff when patients or documentation are at risk of missing a care management milestone.
- Use an EHR registry or AI-enabled platform (like Casey) to:
- Why Casey Matters:
- In rural clinics where clinicians juggle multiple roles, Casey’s automation reduces administrative burden, improves billing accuracy, and maximizes revenue capture.
- By ensuring no minute of non-face-to-face care and no eligible code is overlooked, Casey frees up staff to focus on quality patient care and reducing avoidable hospitalizations.
Final Thoughts
Chronic Care Management represents a powerful opportunity for RHCs and FQHCs to improve outcomes for high-risk rural patients while also generating sustainable revenue. As Medicare shifts from a single G0511 payment to granular CPT codes in 2025, clinics that proactively optimize workflows and documentation will be best positioned to thrive.
An AI Case Manager like Casey can serve as the engine that powers this transformation, automatically identifying patients, generating care plans, tracking minutes, and prepping claims so that your team spends less time on paperwork and more time on patient care.
Ready to see how Casey can help your RHC or FQHC capture every dollar of CCM reimbursement (and beyond)?
Reach out today for a live demo, and let’s build a healthier rural future together.
Source